What is mitral regurgitation?
Incomplete closure of the mitral valve during cardiac contraction causes blood to return from the ventricle to the atrium, causing shortness of breath and heart failure in the long run. Know its symptoms and treatment.
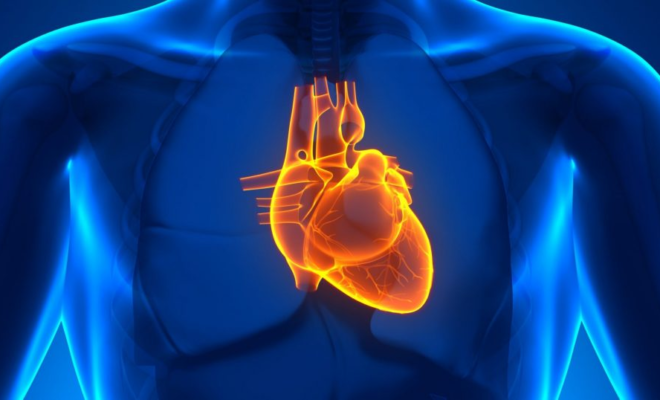
The heart consists of four chambers known as the atria and ventricles. The left atrium and left ventricle are communicated by the mitral valve, while the right atrium and ventricle by the tricuspid valve. When the mitral valve does not close properly, blood backs up from the left ventricle to the left atrium during ventricular contraction or systole. This makes the blood volume that should go out to the rest of the organs return to the left atrium. It’s mitral regurgitation.
But the mitral valve is not just a gate. It is made up of the valves or leaves, which open and close during the cardiac cycle, and some papillary muscles that move them using tendon cords. All of this is a valve apparatus. Any of these components can fail in its mission, determining that the valve’s function is lost, it becomes insufficient.
For many years, while rheumatic fever was prevalent due to pharyngeal streptococcal infections, the mitral valve was frequently affected by this process. In recent decades, the appropriate use of antibiotics in these infections has lowered rheumatic fever in the list of mitral regurgitation causes. However, in the latest registries of cardiovascular surgery societies, it is estimated that mitral valve pathology only occupies around 35% of cardiac operations due to valve causes, being much higher than those caused by the aortic valve (more than 60 %).
The longer life expectancy has also led us to attend to other reasons why the valves degenerate because the heart undergoes anatomical variations over the years and other diseases such as hypertension, which can dilate the ventricle and finally widening the valve space making it incompetent.
It has always been a frequent cause of murmurs. The development of new technologies such as ultrasound of the heart has also allowed a more precise and perhaps an earlier diagnosis of these types of conditions, thus facilitating better management of symptoms and treatments—both medical and surgical for these patients with mitral regurgitation.
Causes of mitral regurgitation
For many years rheumatic fever has been the main cause of mitral regurgitation. This was a secondary involvement of the mitral valve due to a bacterial infection produced mainly by streptococci.
In the Western world, this process is rare in people under 40-45 years of age due to the best and most widespread use of antibiotics for pharyngeal processes during childhood and adolescence.
Currently, mitral valve prolapse and ischemic heart disease are the main factors that trigger mitral regurgitation. The chordae tendineae are part of the mitral valve apparatus, being found with a greater length in some processes such as myxomatous degeneration, that is, a greater laxity of said chords that cause a deficient closure of the valve due to a loss of tension. This process is called mitral valve prolapse and currently accounts for more than 40% of mitral regurgitation causes.
In the case of ischemic heart disease, when the blood supply to the muscles that tension the chordate tendineae is interrupted or deficient, as can occur in a heart attack, these can rupture and cause acute mitral regurgitation. It is important to emphasize that the acute process, in this case, will cause more abrupt symptoms and a worse prognosis. This mechanism represents approximately one-tenth of the cases.
Other causes of mitral regurgitation are endocarditis (infection of the valves as a result of blood infection or bacteremia from another focus), which represents around 3% of cases; hypertrophic cardiomyopathy left ventricular dilation as a consequence of hypertrophy due to arterial hypertension, and more rarely, idiopathic ruptures of the papillary muscles, some congenital heart diseases and autoimmune diseases ( rheumatoid arthritis, lupus ).
The consequence of all these processes is a return of blood from the ventricle to the atrium, overloading it with a volume of blood that would not correspond to it. Secondarily and retrogradely, it is transmitted to the pulmonary circulation, increasing its pressure and generating pulmonary congestion.
Symptoms of mitral regurgitation
To describe mitral regurgitation symptoms or that accompany this disease, we must distinguish how the regurgitation occurs. Thus, acute insufficiency, generally secondary to an ischemic process such as a heart attack, will cause an acute condition due to papillary muscles’ rupture. This symptomatology is going to present in the form of dyspnea or shortness of breath, sudden, progressive, secondary to pulmonary congestion by fluid. To a lesser degree, we will speak of heart failure, leading to acute lung edema (puddling of the lungs).
In addition to dyspnea, the individual will be unable to remain in the supine position, with greater respiratory distress due to the fluid distribution occupying more lung space.
In the case of other mechanisms, such as mitral valve prolapse or endocarditis, mitral regurgitation symptoms may not appear for years. It is a gradual or chronic process in which the affected individual will notice said dyspnea with certain efforts, less and less until at some point a picture of heart failure occurs (dyspnea, fluid retention in the legs or edema, decreased blood pressure). Urine volume during the day, etc.).
They may also present asthenia or fatigue, with a lower tolerance to basic physical activity in their day-to-day life. Patients with valve prolapse may also have palpitations and chest pain.
If, over the years, mitral regurgitation gradually dilates the left atrium due to the overload of blood that it causes, an arrhythmia known as atrial fibrillation can develop. Both processes will increase the risk of embolism to other organs, mainly the brain ( stroke ), although with less risk than in other valve conditions such as mitral stenosis.
On the other hand, it is characteristic that the doctor, when auscultating with the stethoscope, finds a murmur during systole in patients with mitral regurgitation.


